Using magnetic resonance imaging (MRI) in infants with older siblings with autism, researchers from around the country, including the University of Minnesota (UMN), were able to predict which infants would later meet criteria for autism spectrum disorder (ASD) at two years of age, with 80 percent accuracy.
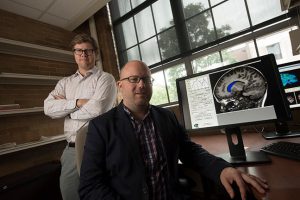
“This area of research is incredibly exciting because it provides an opportunity to understand how autism unfolds early in life,” said Jason Wolff, Ph.D., an assistant professor in educational psychology at UMN and a study co-author. “It provides new clues about the timing and specific mechanisms of brain development that precede a diagnosis. It also offers the unprecedented possibility of predicting whether or not a child will develop autism based on neurobiological data.”
“Typically, the earliest an autism diagnosis can be made is between ages two and three. But for babies with older autistic siblings, our imaging approach may help predict during the first year of life which babies are most likely to receive an autism diagnosis at 24 months,” said senior author Joseph Piven, M.D., the Thomas E. Castelloe Distinguished Professor of Psychiatry at the University of North Carolina-Chapel Hill.
This research project included hundreds of children from across the country and was led by researchers at the Carolina Institute for Developmental Disabilities (CIDD) at the University of North Carolina (UNC). The project’s other clinical sites included the University of Washington, Washington University in St. Louis, and The Children’s Hospital of Philadelphia. In addition to the University of Minnesota College of Education and Human Development, other key collaborators are McGill University, the University of Alberta, the College of Charleston, and New York University (see ibisnetwork.org for more information.)
For this study, published today in Nature, the team of researchers conducted MRI scans of infants at six, 12 and 24 months of age. They found that the babies who developed autism experienced a hyper-expansion of brain surface area from six to 12 months, as compared to babies who had an older sibling with autism but did not themselves show evidence of the condition at 24 months of age. Increased growth rate of surface area in the first year of life was linked to increased growth rate of overall brain volume in the second year of life. Brain overgrowth was tied to the emergence of autistic social deficits in the second year.
The researchers then took these data – MRIs of brain volume, surface area, cortical thickness at 6 and 12 months of age, and sex of the infants – and used a computer program to identify a way to classify babies most likely to meet criteria for autism at 24 months of age. The computer program developed the best algorithm to accomplish this, and the researchers applied the algorithm to a separate set of study participants.
The researchers found that brain differences at 6 and 12 months of age in infants with older siblings with autism correctly predicted eight out of 10 infants who would later meet criteria for autism at 24 months of age in comparison to those infants with older ASD siblings who did not meet criteria for autism at 24 months.
According to the researchers, the findings may have implications for early detection and intervention in children who have older siblings with autism before a diagnosis is typically established. Diagnosis of ASD typically occurs after 24 months of age, the earliest time when behavioral characteristics of ASD can be observed. Intervening early could lead to improved outcomes, as the brain is more malleable in the first years of life compared with later in childhood.
“The findings lay the foundation for the field to move toward attempting to implement interventions before the symptoms that define autism consolidate into a diagnosis,” said study co-author Jed Elison, Ph.D., an assistant professor in the UMN Institute of Child Development.
“Much of what we do as a field to help individuals with autism is reactive,” Wolff said. “We wait for children to fall behind before providing an intervention. We may now be able to find ways to prevent that from ever happening.”
The National Institutes of Health funded this study.
See media coverage of this story in the Star Tribune, Minnesota Public Radio, KARE TV, WCCO TV, and KMSP TV.



